Alabama only state where Medicaid won’t cover some breast cancer screening
Lifesaving tests for genes that increase risks of breast cancer still aren’t available to Alabama Medicaid recipients, despite a push by advocates who say the agency should offer the screening available in all other states.
A study published last year in the journal Healthcare identified Alabama as the only Medicaid program in the nation that did not cover tests for the two most well-known genes that increase breast cancer risk: BRCA1 and BRCA2. Although the state recently added coverage for testing at hospital labs, advocates say the program still doesn’t cover third-party labs that do most testing for breast cancer genes.
Tina Hodge wrote a letter in October 2021 urging the state to add coverage of BRCA1 and BRCA2 testing to Medicaid. The 52-year-old lives in Millbrook and runs the Carmichael Imaging Center at the Montgomery Cancer Center. She also found out in 2015 that she carries the BRCA2 gene.
“I think everybody deserves to have this testing, not just people on private insurance,” Hodge said.
In her letter, Hodge said the lack of testing for people on Medicaid could result in later diagnoses and worse outcomes for those unable to afford private coverage.
Hodge didn’t expect to test positive when she offered to be a guinea pig for her employer as they piloted a genetic counseling program. Her father and uncle had died from pancreatic cancer, but she did not have a family history of breast or ovarian cancer.
Hodge met with a genetic counselor and opted for preventive surgery to remove her ovaries and breasts after she got her results. As she approaches the same age her father died, she will also undergo extra screening for pancreatic cancer.
Lisa Schlager, vice president of public policy for Facing Our Risk of Cancer Empowered (FORCE) said her organization has done extensive research about coverage for genetic testing.
“We’ve done an analysis of what the different Medicaid programs cover,” Schlager said. “To my knowledge, Alabama is the worst offender. Basically, it is the only state Medicaid program in the U.S. that does not cover any sort of genetic testing for hereditary cancer or cancer risk.”
Melanie Cleveland, a spokesperson for the Alabama Medicaid Agency, said the program provides some coverage now.
“Medicaid covers the BRCA 1 & 2 genetic tests for outpatient hospital laboratories enrolled with Medicaid,” Cleveland wrote in an email. “Any of these facilities can bill for the tests.”
Schlager said the types of labs covered by the Alabama Medicaid program do no testing for genetic cancer risk.
“Basically, the coverage is for a non-existent service,” Schlager said.
Alexis Heatherly, a genetic counselor at UAB, said she most often uses the labs Ambry Genetics, Invitae and GeneDX. Even if they aren’t covered by Medicaid, she said many labs offer payment plans.
More women in Alabama die from breast cancer than the national average, according to the Kaiser Family Foundation. The disease kills Black women at a higher rate than white ones, despite lower diagnosis rates, studies have found. Breast cancer was the second most diagnosed cancer in the state after lung cancer in 2021, according to the Alabama Department of Public Health.
Researchers identified the BRCA1 gene in 1994 and BRCA2 one year later. Genes cause about 5 to 10 percent of breast cancer cases, and often causes disease in younger women. The genes also increase the risks of ovarian and pancreatic cancers, which are rarer and deadlier than breast cancer.
Heatherly often meets with patients before they have genetic testing and said it can give them more knowledge about how best to approach treatment.
“Sometimes someone might be diagnosed with breast cancer and have two different options for surgery,” Heatherly said. “Maybe their providers offer and lumpectomy or bilateral mastectomy. They may have higher risks of a second primary breast cancer, so even though they may be eligible for that breast-sparing surgery like a lumpectomy, often times these patients if it comes back positive may elect to have that bilateral mastectomy.”
The Affordable Care Act increased access to testing and counseling for breast cancer genes for people with family histories of cancer or other risk factors. Medicare, the program for older Americans and those with disabilities, covers testing for some people diagnosed with cancer.
State Medicaid programs have different coverage requirements. Most cover both testing and genetic counseling for BRCA1, BRCA2 and Lynch Syndrome, a hereditary form of colorectal cancer. After North Carolina started covering genetic testing in 2021, Alabama was the last state without coverage for its Medicaid population. It is one of six states that don’t offer testing for Lynch Syndrome.
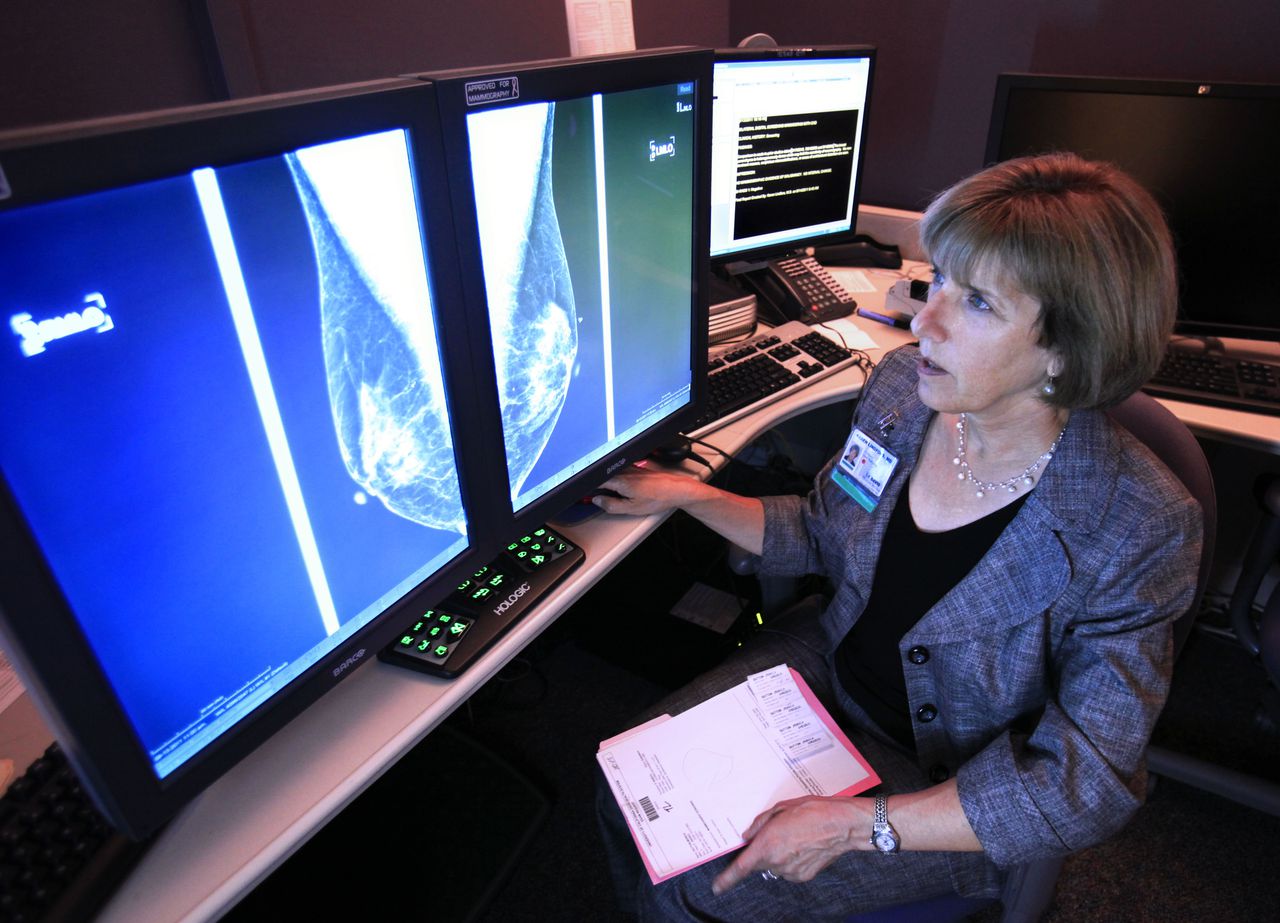
Schlager said state Medicaid programs that cover testing for breast cancer genes tend to also cover additional screening patients need to prevent advanced cancer. Those procedures, which can include mammograms, MRIs and colonoscopies, can be much more expensive than genetic tests.
Alabama has a free breast and cervical cancer screening program for low-income women, but it only offers access to mammograms, PAP smears and clinical follow up. It does not offer free or low-cost genetic testing.
Most Medicaid programs also cover genetic counseling in addition to testing, so patients understand their risks and take action to prevent cancer. Heatherly said individuals with rare cancers in the family and those who have been diagnosed with breast cancer at a young age could be candidates for genetic screening. Men can also have BRCA1 and BRCA2 genes that increase risk of male breast and pancreatic cancer.
Hodge said it is important for people to know their options after a positive test. People can improve their health by increasing screening or scheduling preventive surgeries. The worst thing is to get test results and do nothing, she said.
“What I tell a lot of people is once you know, you can’t unknow it,” Hodge said.