Time for another COVID-19 shot? FDA considers spring vaccine booster
Seven months have passed since the bivalent COVID-19 booster was first made available. Is it time for a springtime jab?
Immunosuppressed people and the elderly — two groups who are particularly vulnerable to severe COVID-19 — are asking their doctors that question.
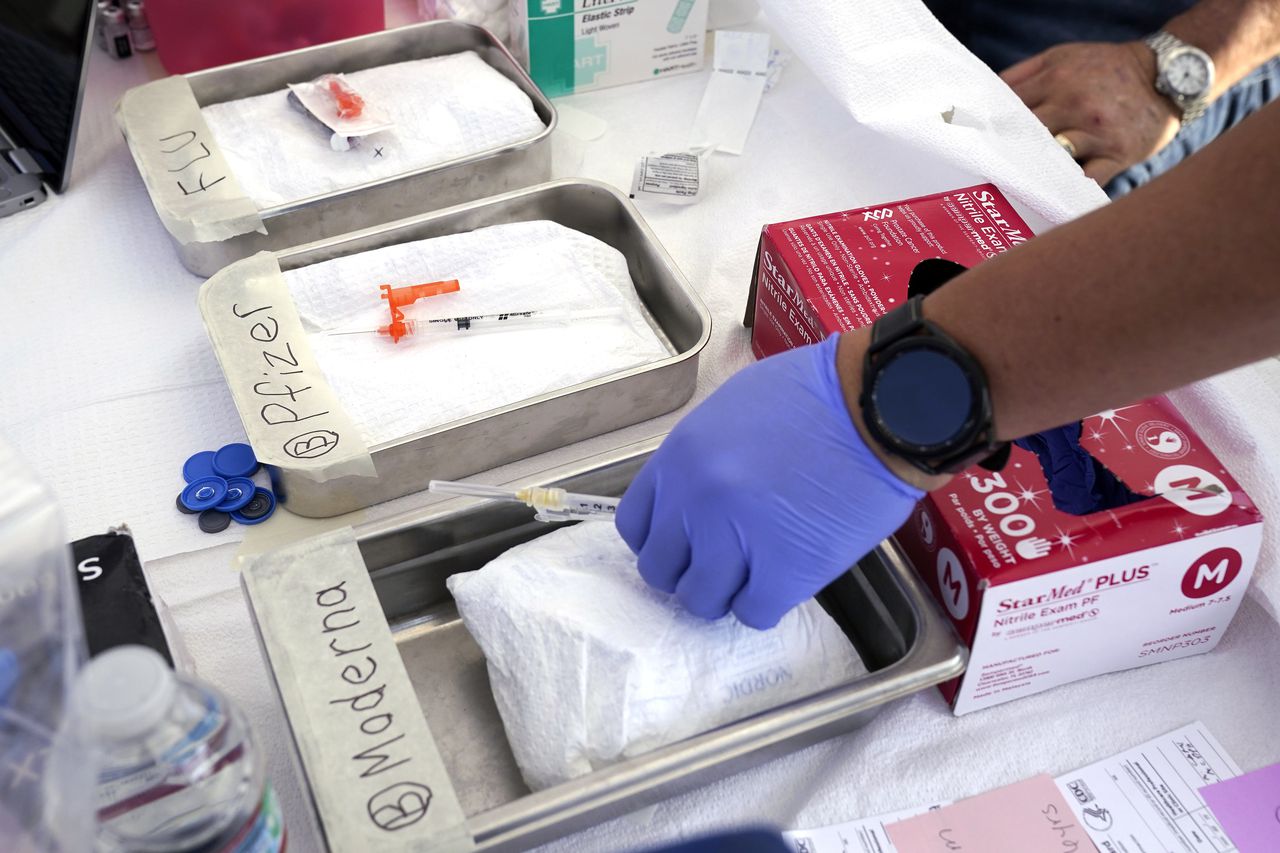
Thus far, the U.S. Food and Drug Administration has authorized only one booster dose of the newest formulations of the vaccines, called a bivalent shot that’s tailored to protect against the COVID-19 omicron variant.
In regards to a possible spring booster, the FDA has said that it continues to “closely monitor the emerging data in the United States and globally, and we will base any decision on additional updated boosters upon those data.”
Some immunosuppressed patients may decide, after consulting their physician, to get a second bivalent shot, said Dr. Steven Gordon, chairman of the department of infectious disease at the Cleveland Clinic. Immunosuppressed people have weakened immune systems, due to illness or medications, and are not able to fight off all infections as easily as healthy people.
“If you’re immunosuppressed and six months from your last bivalent booster, would you benefit from getting another booster? There is no guidance on that,” Gordon said. “Some people are choosing to get re-upped (with a second bivalent) immunization at six months. But remember, we try to do this data driven. Just because we have something, if it’s not effective, you really don’t want to give it. I think that’s the conundrum.”
The situation is different in Canada and the United Kingdom. In those countries, health officials have offered, but not recommended, that the elderly and immunocompromised get a booster COVID-19 shot six months after the last dose.
Currently, Americans who want to be fully vaccinated against COVID-19 have to first get their primary vaccinations — two shots of the original vaccine spaced weeks apart. That’s followed at least two months later by a booster, currently the bivalent booster shot that’s tailored to protect against the omicron variant.
The FDA in January announced that under a new approach coming this fall, most people will be advised to simply get the latest vaccine annually each fall, like the influenza shot. People who still need to receive two doses initially, such as young children and older people, will use the same formulation for all three shots.
The World Health Organization released a preliminary report in late March stating that only people at high risk of severe COVID-19 need additional boosters, and the immunocompromised will need booster shots more frequently.
Meanwhile, it seems clear that even if a spring booster were recommended, many American adults would ignore the health advice, since they never bothered to get the first booster.
Nationally, only 55 million Americans have received an updated COVID-19 booster dose, out of a population of more than 334 million, according to the CDC.
For most immunocompromised people, vaccine protection fades in just a few months, health experts said. That’s why an FDA decision about spring COVID-19 boosters could be especially important to people with weakened immunity systems, as well as the elderly.
About 53 million adults age 65 and older live in the United States, making up about 16% of the population, according to the Census Bureau.
And 7 million Americans have weak immune systems because of an illness or a medication.
Hybrid immunity protects the young, healthy
The question of whether there will be a spring round of COVID-19 booster shots is less urgent for young and healthy Americans, health experts said.
So many people have recovered from COVID-19, there is less need for boosters among this cohort, heath experts say.
“Hybrid immunity” is a combination of protection from vaccines and infections. Multiple studies suggest it is better against infection, and especially against severe disease, than infection or vaccination alone.
COVID-19 hospitalizations of young people have decreased because they are likely to have hybrid immunity and strong immune systems, and are less likely to have co-morbidities that affect their immune systems.
By February 2022, almost 60% of the U.S. population, including 75% of children, had had COVID-19, according to the CDC.
In December 2022, an analysis of 26 studies, published in the journal Lancet Infectious Diseases, found that 1 year after vaccination, hybrid immunity conferred about 42% protection from infection in adult populations and 97% protection from hospitalization or severe illness. That as compared with 25% and 75%, respectively, 1 year after infection alone.
People with hybrid immunity, the study authors wrote, “might be able to extend the period before booster vaccinations are needed compared to individuals who have never been infected.”