Since there’s a war on sex ed, here are 5 ways to have safer sex for National Public Health Week
The best sex is safe sex. If you had a lackluster sexual education (just a little over a third of American high schools teach sex ed that aligns with CDC standards, you may be confused about how to keep sex safe. And with the continued attack on sex education from conservatives, this important information is becoming harder for young people to access.
For National Public Health Week, Reckon is sharing some advice from sex educators about how to keep sex safe along with resources about how to educate your peers, kids and partners.
The good news is there are lots of simple ways to prevent sexually transmitted infections and pregnancy. Finding the methods that work best for you and your partners is the hard part.
We reached out to sex educators Erica Smith and Tia Savonne who both use their Instagram accounts to share more about the work they are doing to improve sex ed and share sex ed tips for people who had (and sometimes memes).
“For people who grew up in purity culture, they are completely unprepared for what they’re going to experience in a sexual encounter,” Smith said, who has been working as a sex educator since 2000. “And in my experience, I think people have a hugely overblown fear of STIs (sexually transmitted infections) and pregnancy that is so far out of the realm of reality. I think the fear that gets instilled in people begins to outweigh the evidence about how effective these preventative measures actually are.”
Having safer sex isn’t as scary or complicated as your early 2000s sex education made it out to be. Here are some of her practical tips for having safer sex:
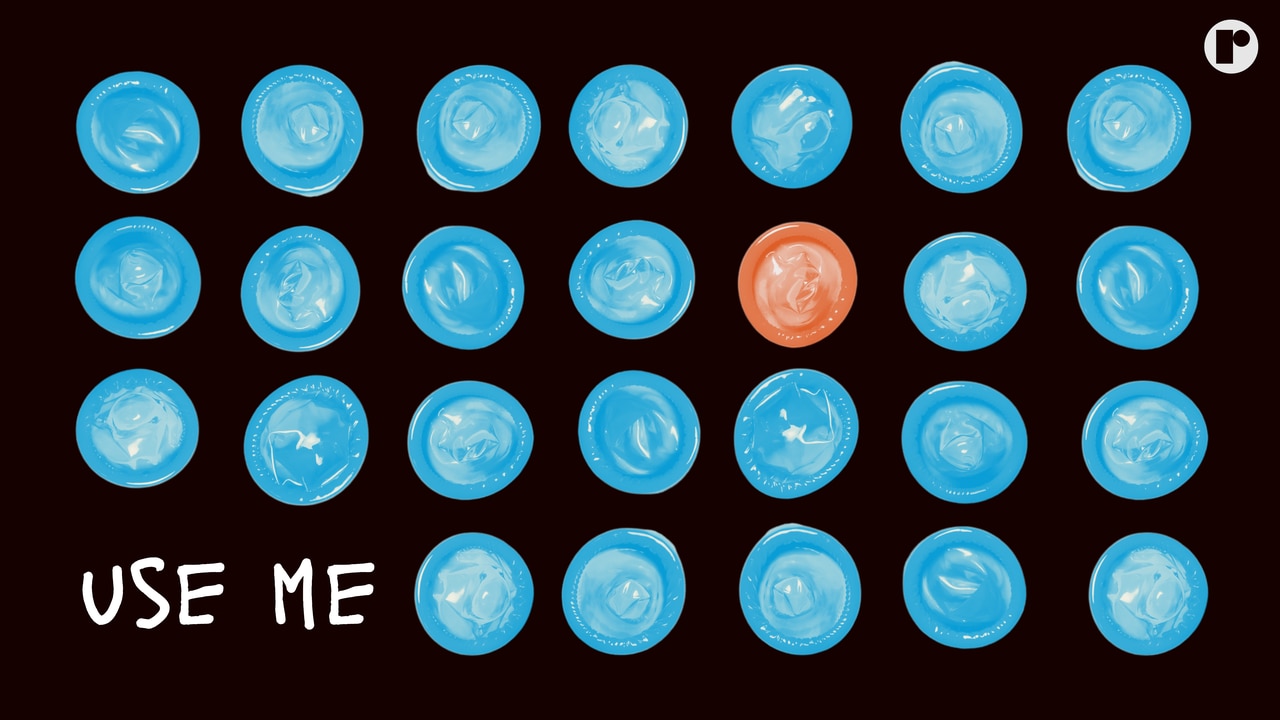
#1 Know how condoms and birth control *actually* work
Abstinence-only sex education, especially religious abstinence-based sex ed, has often included misleading information about condoms and birth control. A common narrative is that condoms aren’t 100% effective at preventing all STIs, which is true, but this skewed fact often leads to a misunderstanding of their effectiveness, Smith said.
“Most of the time when condoms fail, it is because of a human error,” she said.
Here are some quick tips for using an external condom correctly:
- Check the expiration date (don’t use an expired condom)
- Ensure the condom hasn’t been stored at extremely high or low temperatures
- If applying the condom to a penis, make sure to leave room at the tip for semen
- Hold the base of the condom while removing it from your partner to avoid spilling semen or other fluids
- Never re-use a condom
Size does matter with condoms, and if you’re unsure about or if the fit is uncomfortable, consult this chart from VeryWellHealth.
Hormonal birth control is also very effective when used correctly, and while it’s not the best choice for everyone when it comes to preventing pregnancy, it’s still one of the most commonly-used pregnancy prevention tool American women use today, according to the Centers for Disease Control and Prevention.
If a certain “more effective” birth control method doesn’t work for you and your partner, you can consider less risky activities or other ways to mitigate whatever sexual risk you’re hoping to avoid.
“some people do not want to use a condom, no matter what you say. There are people who don’t want to use hormonal birth control. There are a number of reasons why people don’t do things that we want them to do,” she said.
#2 – Know your STI status
Speaking of preventing infections, it’s important to know your own and your partner’s status. There are many resources for free STI testing, even if you don’t have health insurance. You can find a free clinic near you through Planned Parenthood or teensource.org.
Some STIs carry no symptoms, but can still put your partner at risk and cause discomfort and health issues if left untreated. Stigma around STIs remains, so talking about testing may be awkward to discuss with your partner. Here’s Smith’s advice for starting that conversation:
“Hey, our relationship is progressing, and it seems we may consider having sex soon. My sexual health is important to me, so I was last tested for STIs (enter date) at (enter clinic). I was negative for (enter STIs you were tested for). How about you?”
If this conversation doesn’t go well, Smith said she would recommend reconsidering having sex with this person.
If your status is positive…
Having a sexually transmitted infection doesn’t make you dirty or less worthy of affection or sexual intimacy. What do you do if you have an STI that can’t be treated with antibiotics? There are options.
Talk to your partners about your status and discuss what steps you take to keep it to yourself. Keep it factual. Pseudoscience does no good here.
Here are some suggestions for starting that conversation:
“Hey, I want you to know I have HIV, but my treatment makes it undetectable.”
“I have herpes, but that doesn’t mean I can’t have sex with you. I want to talk to you about my doctor’s suggestions for preventing spread.”
Medications like PrEP can protect you from HIV and other treatments can make HIV transmission very unlikely. Not every sexual interaction can spread diseases like herpes. Know the facts about your status and communicate those with your partner, Smith said.
What’s important to remember is that many people living HIV or herpes who are managing their condition have fulfilling sex lives, and often do not spread their conditions to their partners.
#3 – Know your birth control options (and use them properly)
Having the kind of sex that could get you (or your partner) pregnant? There are many hormonal and non-hormonal ways to prevent a pregnancy:
Hormonal: The pill, IUD, implant, patch,
Non-hormonal: Condoms, Cycle tracking
Generally, hormonal birth control methods are more effective at preventing pregnancy, but non-hormonal barrier methods are also very effective at preventing pregnancy and STIs when used correctly.
Birth control is not one-size-fits-all. It’s important to find what works for you and your partner.
#4 – Hygiene
Some simple hygiene goes a long way to prevent infections like yeast infections or bacterial and fungal infections around the genitals—which should not be confused with STIs, but definitely annoyances.
-Wash your hands
-Wash your body
-Wash anything else you are putting near someone else’s genitals
(Hygiene is sexy)
#5 – If you didn’t consent to sexual activity, it’s not safe
Last but certainly not least, let’s talk about consent.
If asking for consent feels awkward, that’s ok. Here are some phrases you can use to ask for consent:
“Can I touch you here?”
“Do you like that?”
“Are you comfortable with this?”
Despite a push toward consent education across the pond in the United Kingdom, former sex education teacher turned sex ed curriculum writer Andrew Hampton said he wants to engage boys on the topic of consent around ages 11 to 13 — before they become sexually active.
The rise of problematic influencers like Andrew Tate, who push the masculinity culture that teaches boys they are superior to girls and pushes back on the fear-based consent education given to boys in the UK.
“If we focus on boys around age 11, in five years, things would be very dramatically different. In 10 years, we’d have a different society altogether, because those boys could have a different perspective on how men are abusing women [in matters of consent],” Hampton said.
“Changing boys perspective means they can decide that talking about girls, as friends and as romantic friends can be done with banter or irony that is controlled and dignified. And boys can enjoy the dignity they have when they talk about girls.”
Consent is clear and enthusiastic. If the person you are with is intoxicated or a minor, they cannot consent.
‘Cause if it ain’t a hell yes, it’s a hell no.
Follow @RAINN to learn more about consent and sexual violence.